Environmental Monitoring: Strategies To Implement Better Practice & Improve Vendor Relationships In Sterile Compounding Facilities

By Engaged Expert
Alex McDanielAlex began his career during 2016 in cleanroom certification where he held both an accreditation for Biosafety Cabinet Certification (NSF/ANSI 49) and as a CETA Registered Certification Professional. Since 2020, he has dedicated his time exclusively to Environmental Monitoring, providing clients with technical support and developing standardized technician training.
Working With A Vendor
Outsourcing EM can save a lot of time and resources- resources that can be spent on running the facility’s day-to-day operations. It is widely known that many contract testing laboratories and certification companies offer on-site “white glove” service to perform routine or investigational monitoring, but the importance of “vetting” a vendor cannot be understated. These professionals provide a service that ultimately the pharmacy is responsible for, so ensuring that a solid relationship exists with the vendor will go a long way to keeping auditors happy – and the pharmacy compliant.
First – ensure the vendor has appropriate credentials to perform microbiology testing for USP <797>. This method will be included in the scope of their ISO 17025 accreditation. This demonstrates that the proper quality systems and procedures are in place to carry out the incubation, enumeration, and identification of organisms in line with current regulations. The qualifications of the technicians must also be reviewed. With the increased focus from the 2022 version of the chapter on showing staff competency, this applies to the vendors, too. The company should have a through and documented training program in place.
After a vendor has been selected, communication is key! Make sure the company understands any potential scheduling requirements that may exist. It is of course most practical to perform surface sampling at the end of a shift, or during the most opportune time based on workload if the facility operates on a 24-hour schedule. If the vendor is scheduled for a morning appointment before the staff begin to compound, the sampling data will not provide the true measure of how the daily disinfection and hand-hygiene practices are functioning. Sampling under dynamic conditions is not only a requirement, but best for patient safety, as it shows the behaviors in the compounding area are continuing to maintain the low levels of bioburden needed under a worst-case scenario.
Once the vendor arrives, having availability to speak with them before and after the service is performed will greatly benefit both parties. Oftentimes, there is not enough communication to understand each party’s process. To build a better relationship, the vendor needs to understand the facility’s material transfer procedures to clean their sampling supplies into the cleanroom suite, as well as the hand-hygiene and garbing steps to properly gown. It is so important to share these procedures because of the responsibility that falls on the sterile compounder to maintain the cleanroom areas.
There may also be more than one sampling plan to execute. Perhaps information specifically on the cleaning and disinfection practices is desired, which would differ in terms of room conditions during sampling and will feature alternate sampling locations for air and surface samples. Ensure that there is a clear understanding of what plan will be utilized.
Proper monitoring takes time to perform correctly- it is an aseptic process, just as compounding is. Make sure the vendor has the time needed to do what they need to do once inside the cleanroom, so they do not feel rushed, resulting in potential sampling mistakes.
Poor communication may result in data that gives an inaccurate representation of the cleanroom’s microbial state of control. Taking time to have these kinds of conversations, will save an e-mail to the vendor when the testing results come in asking “what happened?!”
It has been observed through field experience that some EM plans and programs have not changed over several years. Reviewing this information to assess the plan’s suitability on an annual basis is best to make sure that your locations and sampling methods are appropriate for the type of data that you want to recover.
“To build a better relationship, the vendor needs to understand the facility’s material transfer procedures to clean their sampling supplies into the cleanroom suite, as well as the hand-hygiene and garbing steps to properly gown.”
Reviewing Current EM Procedures
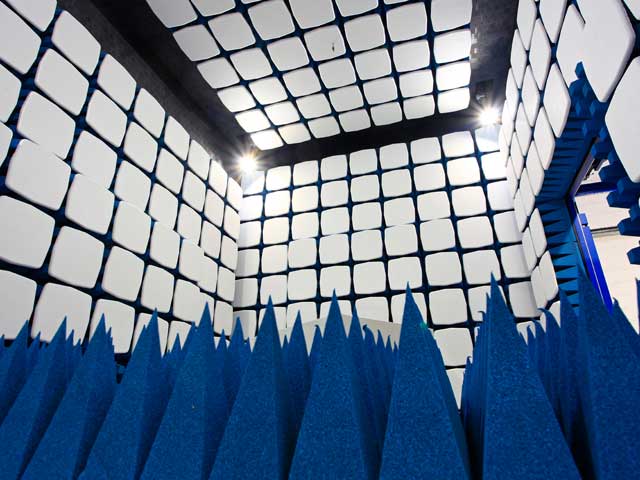
Much has been published about the EM related revisions made to USP Chapter <797> in the 2022 version. It is easy enough to read the chapter to understand what has changed, but what does this really look like inside the cleanroom suite? A few of the more impactful changes are discussed below. Additional regulatory requirements beyond what chapter <797> outlines are not discussed here.
-
There is a “read between the lines” type-change as it pertains to viable air sampling. The language in the revised chapter requires “volumetric air sampling of all classified areas” and is silent about the need to sample the Segregated Compounding Area (SCA), as was included in the 2008 version. While not mentioned, there remains a significant value in monitoring the SCA and Containment SCA (C-SCA), as it could serve as important investigational tool should an excursion occur inside the Primary Engineering Control (PEC). Although the SCA is unclassified, drug products will still be staged in that area before transfer into the PEC.
-
No longer is there a necessity to use fungal-specific media for viable sampling. Previously, the “High Risk” facilities had to meet this requirement, but Tryptic Soy Agar (TSA) is usable for all compounding categories in the revised chapter. Compounders may still be using a two-plate approach (TSA and SDA (Sabouraud Dextrose Agar)), but it may be worth considering a move to a single plate method. If the compounding staff are the ones doing the sampling, they may appreciate cutting the number of plates that they must handle and account for in half by switching exclusively to TSA and – it may be more cost effective too.
Why Are “Best Practices” Really The Best?
Yes, the term “Best Practices” is quite frequently used within the industry, but who is it “best for”? It is best for you, the compounding pharmacy! It is not a sales tactic or intended to make the monitoring process more arduous by exceeding the bare minimums from chapter <797. These concepts exist to achieve things like improved practice, efficiency, reduction of re-work and most importantly- to keep patient safety the number one priority in the pharmaceutical industry.
References:
USP General Chapter <797> Pharmaceutical Compounding – Sterile Preparations (2024)
Find related Resources